Pediatric ECHORN
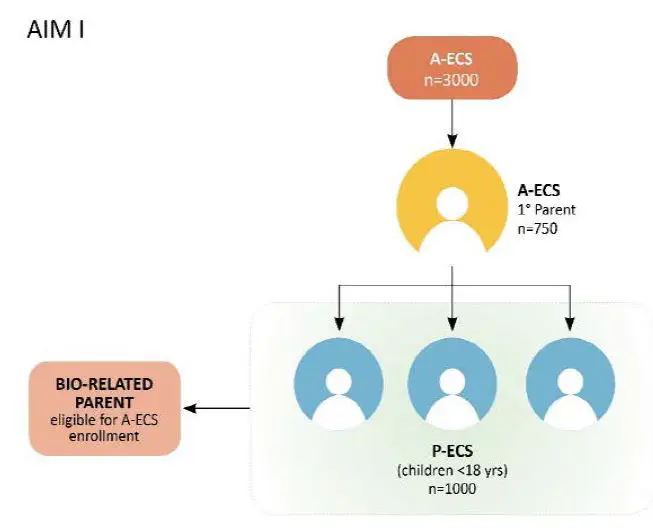 Photo from echorn.org
Photo from echorn.orgPediatric ECHORN
A childhood health cohort for the Eastern Caribbean
The pediatric ECHORN project is a funded NIH programme - full title Pediatric ECHORN cohort study: Intergenerational factors that contribute to cardiovascular risk in the eastern caribbean. It is a follow-on project to the ECHORN adult cohort.
The epidemic of obesity among Caribbean children has been compounded by an increase in other paediatric cardiovascular risk factors such as hypertension and hyperlipidaemia: in the US, among Hispanic and African-descent children, 24.6% and 17.6% have adverse lipid concentrations, and 11.5% and 15.3% have borderline or elevated blood pressure. Increasingly, the effects of sleep deficiency on cardiovascular risk are becoming apparent, another important problem given 45% of adolescents have sleep deficiency, with Hispanic and African-descent children having shorter sleep durations than Caucasian counterparts. This disproportionate prevalence in risk factors among US minority children is likely to worsen adult cardiovascular disease disparities. Interventions to address these conditions in children must be prioritized and based on a thorough understanding of contributors to these trends. The contribution of the adult cardiovascular risk profile (genes, lifestyle, socioeconomic status (SES), neighbourhood disadvantage) to that of the child is recognized as important, but few studies have examined these intergenerational interactions. There is an urgent need to further our understanding of how these intergenerational factors contribute to paediatric cardiovascular risk disparities. In this work, this will be done by exploring the interactions between familial genetics, sleep, and lifestyle factors in determining harmful versus protective cardiovascular risk profiles, to guide the design of targeted and successful interventions to reduce paediatric cardiovascular risk. This five-year project has THREE aims:
- Aim 1: Establish an intergenerational longitudinal cohort study of parents/ grandparents (n=3000) and their children age 5-17years (n=1000), focused on factors that contribute to elevated cardiovascular risk (sleep deficiency, obesity, hypertension, hyperlipidaemia and diabetes). with measures aligning to US cohorts, child participants will undergo a brief physical exam and blood tests. Parents will complete a baseline questionnaire. Sleep actigraphy will provide an objective measure of sleep quality/duration. Blood will be biobanked for future studies investigating the intergenerational impact of genes/ genetic biomarkers on cardiovascular risk.
- Aim 2: Examine the association of sleep duration and sleep quality with lipid metabolism by comparing sleeplipid profiles of parent-child triads with atherogenic lipid levels and protective lipid levels. Sixty index ECS adult parents with atherogenic lipid profiles (elevated non-HDL) and sixty with protective lipid profiles will have their child offspring and their partner recruited. These child/ parent triads will have a comprehensive lipid metabolism panel, biobanking of blood and sleep actigraphy.
- Aim 3: Explore the influence of social determinants of health on paediatric cardiovascular risk (obesity, hypertension, sleep deficiency, hyperlipidaemia). Geographic Information Software will be used to map out the location of adult “cardiovascular hot spots” on each island (areas with clustering of individuals with multiple cardiovascular risk factors). Stakeholder engagement (SE) meetings will discuss how to define the boundaries of these “hot spots” and contributing neighbourhood level factors (e.g. safety, walkability, food environment). Measures for quantifying neighbourhood SES and other SEidentified elements of neighbourhood disadvantage will be developed. This work will inform neighbourhood level interventions to reduce cardiovascular risk.